Online survey of owners' experiences of medicating their cats at home
National Library of Medicine
Samantha Taylor, Sarah Caney, Claire Bessant, Danièlle Gunn-Moore
Abstract
Objectives
The aim of this study was to use an online survey to obtain information from cat owners about their experiences of medicating their cats.
Methods
An online survey containing 35 questions on experiences of medicating cats was circulated to cat owners globally.
Results
In total, 2507 surveys from 57 countries were analysed; 1724 from 'cat owners' and 783 from 'cat owners+' (respondents with significant cat experience, including veterinary professionals). Around half (50.7%) of cat owners were 'sometimes' or 'never' provided with information or advice on how to administer medication; however, 91.8% of those given information found it 'somewhat' or 'very' useful. Around half (53.6%) of owners sought information from the internet about how to administer medication. Total cat owners (cat owners and cat owners+) administered liquids (61.3%), pastes (45.3%) or tablets (39.5%) directly into their cat's mouth; fewer (22.6-24.1%) hid these medications in food. Total cat owners rated tablets significantly harder to administer than liquids; 53.0% chose liquids as their first-choice formulation while 29.3% chose tablets. Insulin injections and 'spot-ons' were significantly easier to administer than any oral medications. Over half (51.6%) of owners reported that medicating their cat(s) had changed their relationship with them; 77.0% reported that their cat(s) had tried to bite or scratch them when medicating. Other challenges included the cat(s) spitting out tablets (78.7%), refusing medication in food (71.7%) and running away (52.7%). Of the owners who failed to complete a course of medication (35.4%), 27.8% stopped near the end of the course, while 19.3% stopped after a few doses, in both cases as medicating was too difficult.
Conclusions and Relevance
Owners appreciate being provided with information about the administration of medication. Frequent challenges when medicating cats include potential human injury and damage to the owner-cat relationship. Pharmaceutical companies should provide a range of formulations to ease compliance. Veterinary clinics should provide information/demonstrations and internet links when prescribing medications.
Happy cats: stress in cats and their carers associated with outpatient visits to the clinic
Journal of Feline Medicine and Surgery
Sarah MA Caney, Natalie J Robinson,
Danièlle A Gunn-Moore and Rachel S Dean
Abstract
Objectives
The importance of the effects of stress on cats is well recognised, with visits to the veterinary clinic a common cause of stress. The aim of this study was to explore owners’ experiences of stress, both for themselves and their cat, during veterinary visits, and to gather data on owners’ perception of resources within the clinic to reduce stress in their cats.
Methods
A questionnaire was used to gather data on cat owner experiences of visits to the veterinary clinic. Data were gathered on the owner’s most recent experience of a consultation, with consultations occurring in February 2020 or earlier coded as a standard consultation, and consultations occurring in March 2020 or later coded as COVID-19 consultations.
Results
A total of 371 responses were received, with 210 coded as standard consultations and 161 coded as COVID-19 consultations. Consultation type varied significantly between standard and COVID-19 consultations (P <0.001), with emergency consultations more frequent and preventive healthcare consultations less frequent during the COVID-19 pandemic. The area in which the owner and their cat waited also varied significantly between standard and COVID-19 consultations (P <0.001), with standard consultations more likely to involve time in a waiting room while COVID-19 consultations were often called straight in or waited outside the practice. Most owners noted behaviours associated with stress in their cats, regardless of consultation type, although trying to hide or escape were noted more frequently for cats seen prior to the COVID-19 pandemic.
Conclusions and Relevance
The findings suggest that outpatient visits to the veterinary clinic were stressful for cats both prior to and during the COVID-19 pandemic, but some measures taken during the pandemic, for example less use of waiting rooms, could be used alongside existing cat friendly measures to help to reduce stress in feline patients.
Veterinary surgeons’, veterinary nurses’ and owners’ experiences of feline telemedicine consultations during the 2020 COVID-19 pandemic
British Veterinary Association
Sarah M. A. Caney,Natalie J. Robinson,Danielle A. Gunn-Moore,Rachel S. Dean
Abstract
Background
There has been increasing provision of veterinary telemedicine consultations, particularly during the COVID-19 pandemic; however, little evidence currently exists examining these remote consultations. The aim of this cross-sectional study was to explore veterinary and cat owner experiences of telemedicine consultations during the pandemic.
Methods
Two questionnaires, one aimed at veterinary professionals and one at cat owners, were launched in September 2020. Questions explored the type of consultation conducted remotely, the perceived advantages and disadvantages of telemedicine, and the role of telemedicine in the future of veterinary practice.
Results
Responses were received from 242 veterinary professionals and 98 owners with experience of telemedicine. Monitoring and advice consultations were felt to be most suited to telemedicine. Reduced stress for owners/cats was seen as an advantage of telemedicine, while lack of clinical examination and risk of misdiagnosis were viewed as disadvantages. Most respondents (85.7% [n = 84/98] of owners; 67.4% [n = 163/242] of veterinary professionals) felt practices should continue to offer telemedicine consultations.
Conclusion
With increasing pet ownership and practice workload, telemedicine may play a crucial role in the future of veterinary practice. Future work should focus on a strategic approach to feline telemedicine, integrating it alongside face-to-face visits and developing technologies to maximise its advantages.
Quality of life and response to treatment in cats with hypersomatotropism: the owners’ point of view
Journal of Feline Medicine and Surgery
Andrea Corsini, Stijn JM Niessen, Diego D Miceli, Sarah Caney, Florian K Zeugswetter, Nadja S Sieber-Ruckstuhl, Carolina Arenas, Linda M Fleeman, Rodolfo O Leal, Martina Battellino, Federico Fracassi
Abstract
Objectives
The aim of this study was to collect clinical information from owners of cats with hypersomatotropism (HS) distributed worldwide, assessing the impact of HS and its treatments on cats’ quality of life (QoL) and survival time.
Methods
A survey focused on clinical presentation, diagnostic procedures, treatments, cats’ QoL and disease progression was distributed worldwide to owners of cats with HS. The owner’s perception of the cats’ QoL before and after or during treatment was defined using a score ranging from 1 (poor) to 5 (excellent). Improvement following treatment (IFT) was quantified using a score ranging from 1 (absent) to 5 (obvious). Different treatment groups, including at least five cases, were compared.
Results
A total of 127 cats were included from at least 11 different countries. Among these, 120 (95%) were diabetic and 7 (5%) were not. Out of 120 diabetic cats, 55 (46%) were treated with insulin as a single treatment (INS). Other treatments were not mentioned to owners in 35/120 (29%) cases. The median QoL score at diagnosis was 2 (range 1–5) and improved after treatment in all groups. Cabergoline (4; range 1–5), radiotherapy (4; range 2–5) and hypophysectomy (5; range 4–5) showed better median IFT scores compared with INS (3; range 1–5) (P = 0.046, P <0.002 and P <0.0001, respectively). Hypophysectomy IFT proved superior to cabergoline (P = 0.047) and was equal to radiotherapy IFT (P = 0.32). No difference was found between cabergoline and radiotherapy IFT (P = 0.99). The median survival time (MST) was 24 months (range 0–75 months). Cats treated with INS showed shorter MST (22 months; range 0–69 months) compared with cats treated with causal treatments combined (36 months; range 3–75 months) (P = 0.04).
Conclusions and relevance
Not all cats with HS will have diabetes mellitus. Causal treatments seem associated with the greatest improvements in perceived cats’ QoL and survival; such treatments should therefore be discussed with owners. Cabergoline could be an effective alternative management option.
Online survey to determine client perceptions of feline chronic lower airway disease management: response to therapy, side effects and challenges encountered
Journal of Feline Medicine and Surgery
Mathieu V Paulin, Sarah MA Caney, Kevin L Cosford
Abstract
Objectives
The first aim of this survey was to report client experiences associated with the administration of common medications, particularly glucocorticoids and bronchodilators, in managing cats with feline lower airway disease (FLAD). The second aim was to ascertain client perception of response to treatment and level of satisfaction.
Methods
This was a prospective cross-sectional study. An online survey was distributed worldwide to cat owners caring for cats with a chronic cough. Only cats reported to have FLAD were included.
Results
A total of 153 complete responses describing cats with FLAD were analyzed. Glucocorticoids and bronchodilators were the predominantly prescribed therapeutics for 140/153 (92%) and 80/153 (52%) of FLAD cats, respectively. Oral and inhalant administration routes were reported most commonly: glucocorticoids (64% oral and 75% inhalant) and bronchodilators (21% oral and 88% inhalant). A review of how air quality could be improved was conducted for 54% of cats. Almost half (43%) of owners reported adverse effects secondary to glucocorticoid administration, the most frequent being polyphagia (26%) and polydipsia (21%). Only 10% of owners reported bronchodilator-associated side effects, with restlessness (9%) being the most common. Difficulties giving glucocorticoid or bronchodilator tablets orally were reported for 33% and 71% of owners, respectively. Glucocorticoid or bronchodilator inhalant therapies were difficult to administer for 28% and 31% of owners, respectively. Frequency and severity of coughing were significantly lower after at least 2 months of treatment, with median numerical input on a slider scale (0–100) of 48 and 42 before, and 10 and 7 after treatment, respectively (P <0.0001). Median numerical input of owner satisfaction was 83%.
Conclusions and relevance
Despite significant improvements in client-reported responses to treatment, challenges associated with the administration of medications and their adverse effects still exist. Promoting awareness of client experiences can facilitate appropriate follow-up, guidance and empathy to further optimize outcomes.
Survey of defecation habits in apparently healthy and chronic kidney disease cats
Journal of Feline Medicine and Surgery
Sarah Jones, Jessica Quimby, Stacie Summers, Sierra Adams, Sarah Caney, Adam Rudinsky
Abstract
Objectives
Changes in bowel movements (BMs) are an important clinical sign in many diseases, including chronic kidney disease (CKD), and the purpose of this study was to collect information on BMs and fecal scores in both apparently healthy and CKD cats. A secondary aim was to assess owner awareness of BM frequency.
Methods
Owners were asked to complete an initial online questionnaire about their cat’s health and litter box habits (including predicted BM frequency and fecal scores) and were then asked to clean the box daily for 7 days and report results (observed frequency of BMs and fecal scores) daily. Differences in BM frequency and fecal scores between apparently normal and CKD cats were compared using the Mann–Whitney test, and predicted vs observed data were compared using the Wilcoxon signed rank test. Difference in percentage of cats defecating more or less than once daily were assessed with Fisher’s exact test.
Results
Survey data from 124 owners of apparently healthy cats and 43 owners of CKD cats who submitted two or more days of daily observations (in addition to the initial questionnaire) were analyzed. Eighty-five percent of apparently healthy cats were observed to defecate one or more times per day and 15% defecated less than once per day. Fifty-eight percent of CKD cats defecated one or more times per day and 42% defecated less than once per day. A significantly higher percentage of CKD cats defecated less than once per day in comparison with apparently healthy cats (P <0.0001). Observed BM frequency was significantly less in CKD cats compared with healthy cats (P = 0.02). Observed fecal scores were not significantly different between healthy and CKD cats.
Conclusions and relevance
The observed BM frequency of cats with CKD was less than apparently healthy cats and represents a clinically important variation from normal.
Prevalence of Disease and Age-Related Behavioural Changes in Cats: Past and Present
Vet. Sci. 2020, 7, 85; doi:10.3390/vetsci7030085
Lorena Sordo, Craig Breheny, Vicky Halls, Amy Cotter, Camilla Tørnqvist-Johnsen, Sarah M. A. Caney and Danièlle A. Gunn-Moore
Abstract
(1) Background: age-related changes in behaviour and health may be thought of as “normal” ageing; however, they can reflect under-diagnosed, potentially treatable, conditions. This paper describes the prevalence of age-related behavioural changes and disease in two UK cat populations at separate time-points.
(2) Methods: owners of cats aged ≥11 years completed questionnaires in 1995 (cohort 1: n = 1236), and from 2010–2015 (cohort 2: n = 883).
(3) Results: the most important behavioural changes in these cats were increased affection towards their owners (reported by 51.9% in 1995; 35.8% in 2010–2015), increased vocalisation (63.5%; 58.9%, respectively), particularly at night (32%; 43.6%), and house-soiling (29.3%; 55.8%). Most (79.4%; 81%) of the cats had visited a veterinary surgeon since becoming 11 years old. The main reasons, aside from vaccinations, were dental disease, renal disease and lower urinary tract disorders in 1995, and dental disease, renal disease and hyperthyroidism in 2010–2015. All major diagnoses were reported significantly more frequently in 2010–2015 than in 1995; behavioural changes were variably associated with these diseases.
(4) Conclusion: elderly cats display age-related behavioural changes and develop diseases that may be under-diagnosed. Veterinarians need to ask owners about these behavioural changes, as they may signify manageable conditions rather than reflect “normal” ageing.
Priorities on treatment and monitoring of diabetic cats from the owners' points of view
J Feline Med Surg. 2019 Jun 26:1098612X19858154. doi: 10.1177/1098612X19858154. [Epub ahead of print]
Albuquerque CS1, Bauman BL2, Rzeznitzeck J3, Caney SM4, Gunn-Moore DA1.
Author information
1 Royal (Dick) School of Veterinary Studies and The Roslin Institute, University of Edinburgh, Easter Bush Campus, Roslin, UK.
2 Equine Medical Services, Yelm, WA, USA.
3 Lohbecker Straße 9, Bersenbrück, Germany.
4 Vet Professionals Ltd.

OBJECTIVES:
The aims of this study were to evaluate: owners' perceptions and priorities on the treatment and monitoring of feline diabetes mellitus (DM); the perceived effectiveness of the communication between veterinarians and clients regarding disease management; and the impact DM has on the owners' everyday lives and human-pet bonds.
METHODS:
An initial questionnaire, then an adapted second questionnaire, were available to owners of cats with DM on vetprofessionals.com .
RESULTS:
A total of 748 questionnaires were completed. At diagnosis, fewer than half of veterinarians discussed how to recognise unstable diabetes (46%) or home blood glucose monitoring (HBGM) (40%). Owners were disappointed that the importance of diet on diabetic remission/stabilisation and HBGM were not discussed. Only 49% of respondents were supervised by a veterinarian/veterinary nurse while first drawing up insulin and injecting their cat. Websites/online forums that owners found themselves were most useful when learning about their cat's diabetes (76% agreed). Over a third of cats (39%) were not fed a 'diabetic' diet but, impressively, 71% of owners used HBGM. Initial concerns about costs, boarding, the effect on their daily life and potential negative impact on the human-pet bond reduced significantly after initiating treatment (P <0.0001).
CONCLUSIONS AND RELEVANCE:
Caring for a diabetic cat requires significant owner commitment, plus support by the veterinary team for the owner and their cat. It is difficult to discuss all aspects of this complex disease with the owner in a single consultation; hence, it is important to involve the entire veterinary team in owner education and provide owners with informative material (eg, useful websites, printouts). Understanding owners' priorities, fears, and which monitoring methods have helped others, is paramount to achieve owner compliance and satisfaction, and so improve the health and welfare of diabetic cats. This study provides useful information on the management of feline DM, which can be instrumental in educating future owners.
Survey of owner subcutaneous fluid practices in cats with chronic kidney disease
J Feline Med Surg. 2018 Oct;20(10):884-890. doi: 10.1177/1098612X17732677. Epub 2017 Sep 26.
Cooley CM1, Quimby JM1, Caney SM2, Sieberg LG1.
Author information
1 Department of Clinical Sciences, College of Veterinary Medicine and Biomedical Sciences, Colorado State University, Fort Collins, CO, USA.
2 Vet Professionals Ltd.
Objectives
The purpose of this study was to survey owners regarding their practices and experiences with the administration of subcutaneous (SC) fluids at home to cats with chronic kidney disease (CKD) to gain insight that might help more owners be successful with the procedure.
Methods
A web-based survey was advertised online. Owners of 468 cats with CKD participated, 399 of whom administered SC fluids. Results Fifty-nine percent of the cats were domestic shorthairs, with >85% of the cats being 10 years of age or older. IRIS stage 3 was most commonly represented (37%). Ninety-five percent of owners said they discussed giving fluids with their veterinarian, with only 42% of those discussions involving additional educational resources. A large majority of owners (85%) said it was either an easy, somewhat easy/no stress or okay experience for them, and a large majority (89%) reported that the experience was easy/no stress, somewhat easy or okay experience for their cats. To increase tolerance, 57% said they gave a treat to their catafterwards, and 60% said they warmed the fluids. Sixty-one percent reported using a 20 G or larger needle, with 49% saying size of needle affected tolerance. Seventy-four percent also felt that the length of time it took to administer fluids affected tolerance. One-hundred milliliters was the most commonly given fluid amount. Hydration status was monitored by 40% of owners by various methods, with 40% of those saying they skipped or added fluids based on hydration assessment. Conclusions and relevance A majority of owners gave positive feedback about their ability to learn and administer SC fluids to their cat wth CKD. Owners reported several strategies that they felt improved tolerance of fluid administration. Overall, the protocol should be tailored to the preference of the cat for best possible long-term success.
In the Eye of the Beholder: Owner Preferences for Variations in Cats' Appearances with Specific Focus on Skull Morphology.
Animals (Basel). 2018 Feb 20;8(2). pii: E30. doi: 10.3390/ani8020030.
Farnworth MJ1, Packer RMA2, Sordo L3, Chen R4, Caney SMA5, Gunn-Moore DA4.
Author information
1 Rural and Environmental Sciences, Nottingham Trent University, Southwell, Nottinghamshire NG25 0QF, UK. Mark.Farnworth@NTU.ac.uk.
2 Department of Clinical Science and Services, Royal Veterinary College, Hatfield, Hertfordshire, AL9 7TA, UK. Lorena.sordo@ed.ac.uk.
3 The Royal (Dick) School of Veterinary Studies and The Roslin Institute, University of Edinburgh, Edinburgh, EH25 9RG, UK. ruoningchen@163.com.
4 The Royal (Dick) School of Veterinary Studies and The Roslin Institute, University of Edinburgh, Edinburgh, EH25 9RG, UK. Danielle.Gunn-Moore@ed.ac.uk.
5 Vet Professionals Ltd. Sarah@vetprofessionals.com.
Changes in the popularity of cat breeds are largely driven by human perceptions of, and selection for, phenotypic traits including skull morphology. The popularity of breeds with altered skull shapes appears to be increasing, and owner preferences are an important part of this dynamic. This study sought to establish how and why a range of phenotypic attributes, including skull shape, affect preferences shown by cat owners. Two questionnaires were distributed on-line to cat owners who were asked to rate preferences for pictures of cats on a 0-10 scale. Veterinarian consensus established the skull types of the cats pictured (i.e., level of brachycephaly (BC) or dolichocephaly (DC)). Preferences were then explored relative to cat skull type, coat and eye color, and coat length. Generalized estimating equations identified relationships between physical characteristics and respondent ratings. Further sub-analyses explored effects of respondents' occupation, location and previous cat ownership on rating scores. Overall, cats with extreme changes in skull morphology (both BC and DC) were significantly less preferred than mesocephalic cats. Green eyes, ginger coat color and medium length coat were most preferred. Current owners of a BC or DC pure bred cat showed significantly greater preference for cats with similar features and significantly lower preference for the opposite extreme. Respondents from Asia were significantly more likely to prefer both BC and DC cats as compared to respondents from other locations. Finally, those in an animal care profession, as compared to other professions, provided a significantly lower preference rating for BC cats but not for DC cats. This work, despite the acknowledged limitations, provides preliminary evidence that preferences for cat breeds, and their associated skull morphologies, are driven by both cultural and experiential parameters. This information may allow for better targeting of educational materials concerning cat breeds.
Attitudes of small animal practitioners toward participation in veterinary clinical trials
J Am Vet Med Assoc. 2017 Jan 1;250(1):86-97. doi: 10.2460/javma.250.1.86.
Gruen ME, Griffith EH, Caney SM, Rishniw M, Lascelles BD.
Author information
1 Department of Clinical Sciences, College of Veterinary Medicine and Biomedical Sciences, Colorado State University, Fort Collins, CO, USA.
2 Vet Professionals, Roslin, UK.
Abstract
OBJECTIVE To determine attitudes of small animal practitioners toward veterinary clinical trials and variables influencing their likelihood of participating in such trials.
DESIGN Cross-sectional survey.
SAMPLE Small animal practitioners with membership in 1 of 2 online veterinary communities (n = 163 and 652).
PROCEDURES An online survey was developed for each of 2 veterinary communities, and invitations to participate were sent via email. Each survey included questions designed to collect information on the respondents' willingness to enroll their patients in clinical trials and to recommend participation to clients for their pets.
RESULTS More than 80% of respondents to each survey indicated that they spend no time in clinical research. A high proportion of respondents were likely or extremely likely to recommend clinical trial participation to clients for their pets when those trials involved treatments licensed in other countries, novel treatments, respected investigators, or sponsoring by academic institutions, among other reasons. Reasons for not recommending participation included distance, time restrictions, and lack of awareness of ongoing clinical trials; 28% of respondents indicated that they did not usually learn about such clinical trials. Most respondents (79% to 92%) rated their recommendation of a trial as important to their client's willingness to participate.
CONCLUSIONS AND CLINICAL RELEVANCE Participation in veterinary clinical trials by small animal practitioners and their clients and patients appeared low. Efforts should be increased to raise practitioner awareness of clinical trials for which patients might qualify. Specific elements of trial design were identified that could be modified to increase participation.
An online survey of dietary and phosphate binder practices of owners of cats with chronic kidney disease
J Feline Med Surg. 2016 Oct 17. pii: 1098612X16672999. [Epub ahead of print]
Caney SM1.
Author information:
1 Vet Professionals Ltd. sarah@vetprofessionals.com
OBJECTIVES:
The objective of this study was to learn about owner experiences of chronic kidney disease (CKD), focusing on use of therapeutic renal diets (TRDs) and intestinal phosphate binders (IPBs).
METHODS:
An online survey was promoted to UK-based cat owners.
RESULTS:
In total, 859 owners participated. Most cats (n = 620; 72.18%) had two or more clinical signs at the time of their CKD diagnosis. Most common were polydipsia (n = 462; 53.78%) and weight loss (n = 426; 49.59%). In 94 cats (10.94%) CKD was only diagnosed as a result of wellness screening. In total, 371 participants (43.19%) reported that their cat's blood pressure had been measured; 100 of these (26.95% of those where blood pressure had been measured) subsequently received anti-hypertensive medication. In total, 90.80% of all participating owners had received a recommendation to feed a TRD. Five hundred and seventy-one owners (66.47%) reported that they were feeding a TRD as a component of their cat's diet. The most common reason for not feeding a TRD was that the cat did not like it (n = 123; 59.13%). Where a veterinary recommendation to feed a TRD had been received, 564 owners (72.31%) reported feeding a TRD as a component of their cat's diet vs seven owners (7.04%) who had not received a veterinary recommendation to feed a TRD. IPBs had been recommended to 321 owners (37.81%) and for 72 owners (8.38%) the recommendation came from a source other than a veterinary professional. Where used, IPBs were commonly added to a TRD (n = 136; 49.28%) and were generally accepted within 4 weeks (n = 178; 73.86%).
CONCLUSIONS AND RELEVANCE:
Awareness of TRDs was high but much lower for IPBs. A veterinary recommendation to feed a TRD was associated with higher compliance.
© The Author(s) 2016.
DOI: 10.1177/1098612X16672999
PMID: 27754938
Flat Feline Faces: Is Brachycephaly Associated with Respiratory Abnormalities in the Domestic Cat (Felis catus)?
PLoS One. 2016 Aug 30;11(8):e0161777. doi: 10.1371/journal.pone.0161777.
eCollection 2016
Farnworth MJ1, Chen R2, Packer RM3, Caney SM4, Gunn-Moore DA2.
Author information:
1 School of Biological Sciences, Plymouth University, Devon, United Kingdom.
2 The Royal (Dick) School of Veterinary Studies and The Roslin Institute,
University of Edinburgh, Edinburgh, United Kingdom.
3 Department of Clinical Science and Services, Royal Veterinary College,
Hatfield, Hertfordshire, United Kingdom.
4 Vet Professionals Ltd.
There has been little research into brachycephalism and associated disorders in cats. A questionnaire aimed at cat owners was used to determine the relationship between feline facial conformation and owner-reported cat management requirements and respiratory abnormalities. Owner-submitted photographs of cats were used to develop novel measures of skull conformation. One thousand valid questionnaires were received. Within these there were 373 valid photographs that allowed measurement of muzzle ratio (M%) and 494 that allowed nose position ratio (NP%). The data included 239 cats for which both measurements were available. Owners reported lifestyle factors (e.g. feeding type, grooming routine, activity level), physical characteristics (e.g. hair length) and other health characteristics of their cat (e.g. tear staining, body condition score). A composite respiratory score (RS) was calculated for each cat using their owner's assessment of respiratory noise whilst their cat was asleep and then breathing difficulty following activity. Multivariate analyses were carried out using linear models to explore the relationship between RS and facial conformation, and lifestyle risk factors. The results showed that reductions in NP% and M% were significantly associated with RS (P < 0.001 and P = 0.026, respectively) and that the relationship was significantly negatively correlated (r = -0.56, P < 0.001 for both). Respiratory score was also significantly associated with increased presence of tear staining (P < 0.001) and a sedentary lifestyle (P = 0.01). This study improves current knowledge concerning cats with breeding-related alterations in skull confirmation and indicates that brachycephalism may have negative respiratory implications for cat health and welfare, as has been previously shown in dogs.
DOI: 10.1371/journal.pone.0161777
PMCID: PMC5004878
PMID: 27574987
An online survey to determine owner experiences and opinions on the management of their hyperthyroid cats using oral anti-thyroid medications
J Feline Med Surg. 2013 Jun;15(6):494-502. doi: 10.1177/1098612X13485481. Epub
2013 Apr 16.
Caney SM1
Author information:
1 Cat Professional, Vet Professionals Ltd. sarah@vetprofessionals.com
Hyperthyroidism is the most common feline endocrinopathy. Treatment options comprise anti-thyroid medication, iodine-restricted diet, surgical thyroidectomy and radioiodine. One hundred and eleven owners of hyperthyroid cats completed a detailed survey asking about their experiences and views on the management of hyperthyroidism. Male cats were slightly over-represented (60 cats, 54%). Concurrent chronic kidney disease was reported in 27% of the cats. Oral anti-thyroid medication was offered to 92% of owners. The final treatment decision was usually based on the veterinarian's recommendation or joint decision-making between the owner and the veterinarian. Almost all of the cats (103, 93%) had received oral anti-thyroid medication at some point in the course of their disease. Sixty-nine cats (62%) were receiving oral anti-thyroid medication at the time of survey completion. Management of hyperthyroidism using UK veterinary-licensed oral anti-thyroid medication (Vidalta; MSD Animal Health, Felimazole; Dechra Veterinary Products) was associated with 72-75% success rates in terms of owner-assessed clinical outcome. The most important treatment priorities for owners were the prescription of the most accurate dose of medication and use of the lowest possible dose. None ranked once-daily treatment as most important to them, and 79% of owners said that they were, or would be, happy to dose their cat twice daily to control its hyperthyroidism. For 62% of owners, pilling their cat twice daily was not a problem. These results suggest that most cat owners are not a barrier to prescribing twice-daily anti-thyroid medication, if required.
DOI: 10.1177/1098612X13485481
PMID: 23591627 [Indexed for MEDLINE]
Feline Nutrition: Results of survey on routine feeding practices of pet cats in 2013
Responder demographics:
- 733 responses from 21 countries
| Country | Responses |
| United Kingdom | 509 (69.4) |
| United States of America | 128 (17.5) |
| Canada | 20 (2.7) |
| Australia | 17 (2.3) |
| Republic of Ireland | 5 (0.7) |
| Central European countries (France, Czech Republic, Germany, Italy, Spain, Portugal, the Netherlands, and Switzerland) |
49 (6.7) |
| Other countries | 5 (0.7) |
| All responses | 733 (100) |
- 30.7% (225/733) of owners had single-cat households.
- 63.2% (463/733) of owners provided adequate nutritional resource capacity for multi-cat households, meaning providing an equal or greater number of feeding stations compared to the total number of cohabiting cats.
- 21.0% of respondents purchased pet food from online suppliers.
The composition of the main ration of pet cats:
- 60.2% of cats were fed combination of wet and dry commercial food.
- 22.6% of cats were fed dry commercial food only.
- 12.0% of cats were fed wet commercial food only.
- 3.7% of cats were fed a home prepared raw meat-based (RMBD) diet.
- 0.7% of cats were fed home produced cooked meat diet.
- 0.7% of cats were fed veterinary prescription diet.
- 0.14% of cats were fed vegan diet.
- No cats were fed a commercially produced raw meat-based diet.
- No cats were fed grain-free diets.
- Higher proportion of pedigree cats were fed a RMBD than non-pedigree cats.
- 97.4%of owners fed their cats treats alongside their main diet.
| Diet | Responses |
| Single component | |
| Commercial dry | 166 |
| Commercial wet | 88 |
| Home produced RMBD | 27 |
| Commercial RMBD | 0 |
| Home produced cooked meat | 5 |
| Veterinary prescription diet | 5 |
| Vegan | 1 |
| Grain-free | 0 |
| Mixed dietary components | |
| Commercial wet and dry | 441 |
| Commercial wet and/or dry and veterinary prescription | 0 |
| Commercial wet and/or dry food with added raw meat | 0 |
| Commercial wet and/or dry food with added cooked meat | 0 |
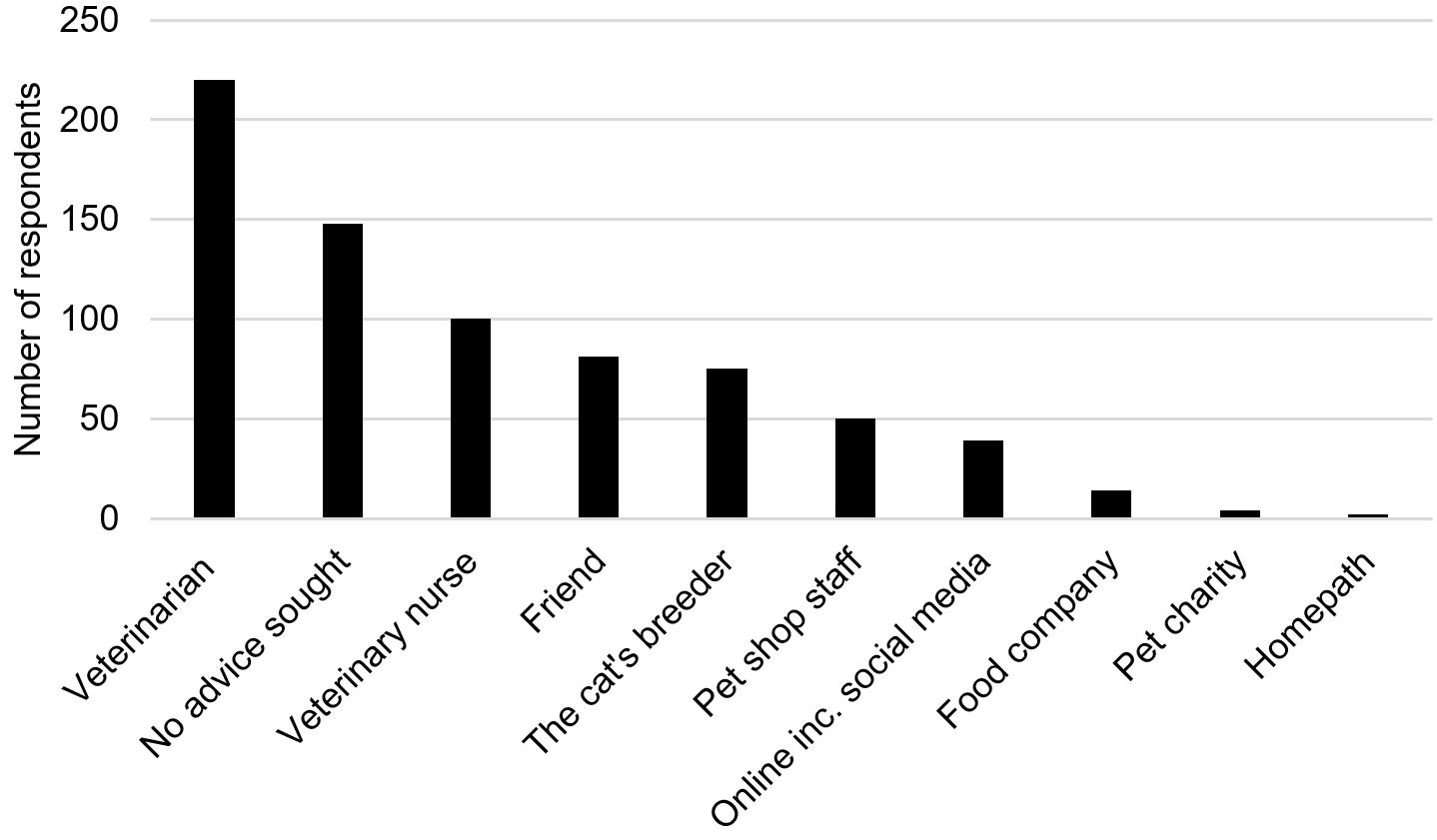
Sources of feline nutritional information study for respondents: